 Workers comp administrators receive 200 to 300 bills a day which need to be directed to adjusters. However, the adjusters don’t necessarily review the bill, even though numerous incidents occur when they are sent out for the wrong reason. Some of these reasons may include a bill for unnecessary treatments, fee schedules changing frequently, or even when an adjuster is unclear of what needs to be paid on a bill.
Workers comp administrators receive 200 to 300 bills a day which need to be directed to adjusters. However, the adjusters don’t necessarily review the bill, even though numerous incidents occur when they are sent out for the wrong reason. Some of these reasons may include a bill for unnecessary treatments, fee schedules changing frequently, or even when an adjuster is unclear of what needs to be paid on a bill.
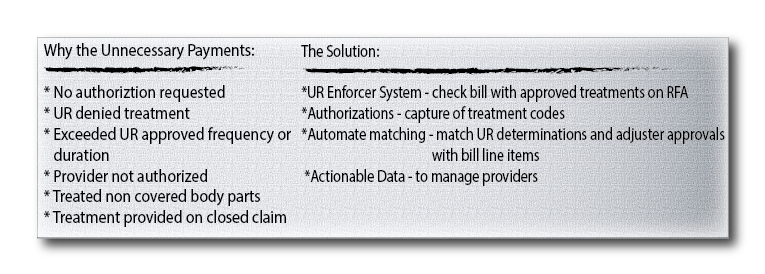
Based on a study conducted by EK Health Services, one database’s library of bills consisted a total of 21% that were sent in error. Among this 21%, half were bills that were sent out for treatment which had not been medically necessary. In addition, some medical providers skip using the Utilization Review process (which actually verifies each case based on state guidelines), and still provide medical treatment with disregard to any authorization for it. On the other hand, there are also providers that will indeed use the Utilization Review process, but still provide treatment when the request is unnecessary or denied. Under scenarios like these, it is necessary for a UR Enforcer to come into play because the application augments traditional bill review savings by verifying bills against treatment authorizations from utilization reviews, and flags the questionable bills for higher level of scrutiny.