Medical Claims Software
DataCare’s AHSHAY! revolutionizes medical claims management as a Medical Process Manager (MPM), designed specifically for adjusters.
Software Built for Workflow Efficiency
Work through your medical claims management process faster and easier. AHSHAY! streamlines your claims tracking and management process by guiding users through each step. Accessed from any type of device, users receive clear indicators for approvals, referrals to Utilization/Preauthorization Review (UR), and adherence to company guidelines. Our innovative tools allow you to annotate bills digitally and track changes in real time, so every important detail is captured and stored.
AHSHAY! medical claims software helps you seamlessly generate and send bills and letters. Access direct email and faxes to maintain compliance at every level. You’ll receive an overarching view of all vital documents, including medical reports, treatment requests, and bills. The advanced functionalities— robust search capabilities, timely alerts, historical data access, and flagging features—greatly boost claims management workflow efficiency. By adopting AHSHAY! as your MPM, you elevate the quality of your service and significantly reduce claims processing costs by at least 25%.
My favorite thing about the system is that reports are automatically sent to those who receive it.
AHSHAY!: Your Medical Claims Software
Our healthcare claims management software is designed to fit seamlessly into the daily routines of nurses, physicians, and adjusters. Users are discovering that it enhances patient care coordination and streamlines their workflow, leading to significant time savings in their daily tasks.
Get More Productive Without More Effort
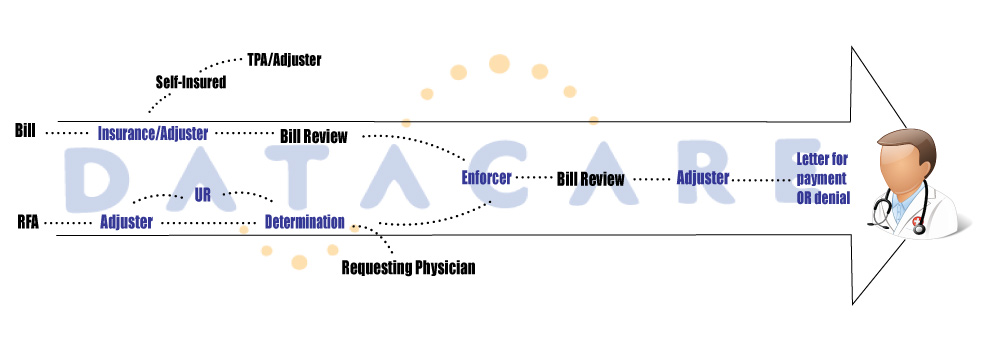
Adjusters have a pivotal role in managing claims. They need a system that helps them increase productivity and visibility when working on a claim. For managers, analytics make sure everyone is on track. AHSHAY! was created for this reason: to optimize the adjuster workflow with immediate communication and tracking, and to provide real-time reporting. DataCare’s solutions — built on the Ahshay! Platform — is a comprehensive system that enables claims tracking through all steps of the process: case management, pre-authorization, utilization/preauthorization review, and bill payment.
Jackie Payne, the Senior Director of Managed Care Operations, is one of our valued clients who implemented AHSHAY! into their organization. Jackie’s goal was to provide top-quality solutions to their clients, and our medical case management system does just that. It enhances the efficiency of their managed care team and facilitates a smooth integration with their bill review platform.
Our investment in the DataCare platform is a part of our ongoing commitment to utilize advanced technology to help clients manage their medical expenses.
Other Success Stories
Ahshay! and its various case management software modules have proven to improve the effectiveness and efficiency for our clients. Here are just a few examples:
Craig Bates & Susan Kennon of Timberline Medical Consultants, said, “Datacare has been an outstanding provider that meets our needs for all providers with no complaints from anyone. They provide ongoing attention for meeting increasing demand for the development of analytical reporting systems specific to our needs. Their staff of customer service, people and engineers have always been eager to help us with those needs. We believe that Datacare is the best case management software available in our industry.”
Michele Settel, President of Ascential Care Partners, emphasized, “DataCare really understands the case management and utilization review ecosystem. Their platform is robust and stable, a must-have in a systems provider. Our focus at Ascential Partners is to promote the right treatment so our patients get back to their lives using the most expedient, cost-effective, and solution-minded way. DataCare is an important partner, helping us with our mission.”
Thomas Kokkines, Vice President of Optimal Case Management, stated, “The reporting offered through Ahshay!, along with the evidence-based data that ODG provides, allows us to paint a clear picture to our clients on how our nurses are positively impacting return-to-work results. The information captured in Ahshay! allows us to analyze various data elements that can be useful to not just our clients, but our nurses and management.”
A Risk Management Supervisor said “The Datacare team is wonderful to work with and is always responsive! They continue to improve the software as well as their caliber of staff. Datacare is the best company I have worked with in a capacity of vendor because they truly care about the quality of their product and service! I would recommend Datacare to anyone looking for claims/bill review software.”
Discover the wide range of applications you can do with AHSHAY!
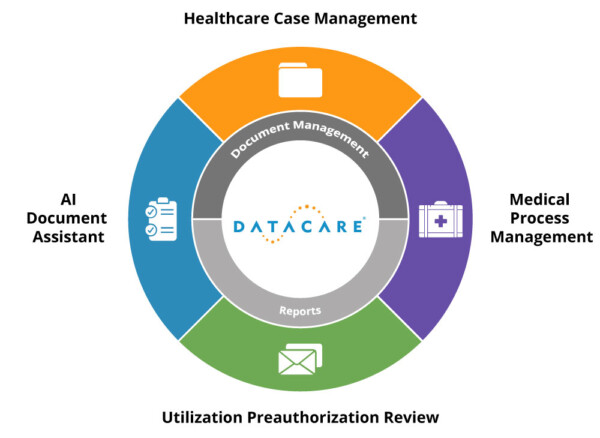
Healthcare Case Management
Designed for healthcare professionals, AHSHAY! is a Nurse Case Management software that simplifies and enhances the workflow. With its customizable reports, accessible from any location, this software empowers professionals to prioritize patient care and alleviate administrative tasks, streamlining their processes and improving overall efficiency.
Beyond this, AHSHAY! also functions as a Workers Comp and Automotive Case Management software.
Utilization / Preauthorization Review
DataCare’s AHSHAY! platform includes a Utilization Review/Preauthorization Software. This module streamlines healthcare workflows by expediting decisions, minimizing redundancies, and ensuring compliance. It directly integrates guidelines, automates tracking, and generates audit-ready reports.
Furthermore, the platform incorporates tracking automation and bill review, enhancing the management of medical processes.
Medical Process Management
AHSHAY! is a Medical Process Manager (MPM). It’s a user-friendly tool designed to assist adjusters in managing the medical review process. By streamlining approvals, integrating guidelines, and ensuring compliance, AHSHAY! effectively lightens the workload and elevates the efficiency of medical claims processing.
AI Document Assistant
Utilizing AI, our AI Document Assistant module efficiently organizes, sorts, and retrieves documents. It intelligently categorizes documents based on content, seamlessly integrating them into relevant case management workflows. This module reduces the need for manual review, streamlining document handling, and improving overall efficiency.